Strategies to Diversify the Medical Student Training Pipeline Into Cardiology
The demographic characteristics of the physician workforce in cardiology are not reflective of the U.S. population. Underrepresentation of women, racial and ethnic minorities, others from low socioeconomic backgrounds, and those with osteopathic and international medical training persists in the field. Professional societies have created pipeline training programs to reduce workforce disparities and enhance clinical outcomes. In 2020, the American College of Cardiology (ACC) convened the Medical Student Leadership Group (MSLG). While serving as inaugural members, we have recognized gaps in the pipeline, including few cardiology mentors from underrepresented in medicine (URiM) groups, inactive cardiology interest groups, and limited exposure of students to cardiology. Based on our experiences, we share 4 strategies in our MAPS paradigm to diversify the pathway into the cardiology workforce: meaningful mentorship, academic exposure, professional development, and a support network (Figure 1).
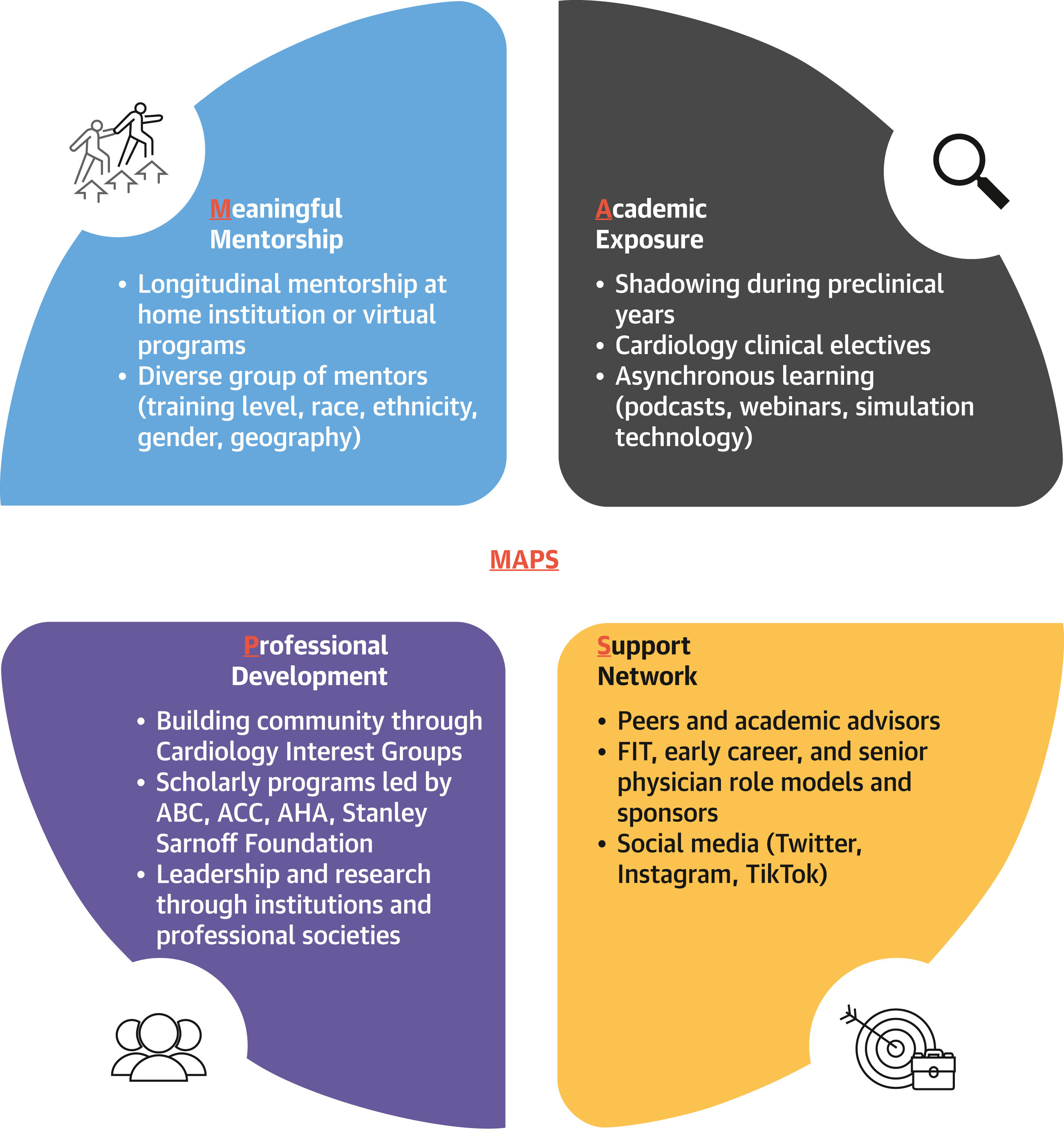
The MAPS Approach to Diversify the Medical Student Pipeline Into Cardiology
The MAPS approach outlines a 4-part strategy to diversify the pipeline into cardiology: meaningful mentorship, academic exposure, professional development, and support network. ABC = Association of Black Cardiologists; ACC = American College of Cardiology; AHA = American Heart Association; FIT = Fellow-in-Training.
In MAPS, meaningful mentorship can enable trainees who report early interest in cardiology to identify faculty member(s) on campus or virtually. For example, trainees whose mentor identifies of the same gender and/or race report a more positive mentorship experience. Likewise, female cardiology fellows who lacked a female mentor were less likely to pursue a career in interventional cardiology. In a third study, longitudinal coaching in a cohort of internal medicine residents increased chances of fellowship placement. We believe having a mentor who fully understands a student’s goals creates powerful mentorship in contrast to random assignment. If this relationship organically forms at an early stage of a student’s training, it is more meaningful than if only at inflection points, such as when applying to residency.
However, meaningful mentorship may need optimization by looping in a third party. For example, societies can help maintain connectivity between mentor and mentee. Last year, the ACC implemented programming among female, Black, and Hispanic internal medicine residents and cardiology mentors. The Association of Black Cardiologists (ABC) has offered a similar mentorship program for college students. At our medical schools, advisors are paired with students through an office of medical education. We believe in formalizing the mentorship process, with or without a third party, with recognition of race and gender for students. Although a limited number of URiM mentors exist, schools and societies should be encouraged to hold sessions for those mentors to share best practices of meaningful mentorship to encourage underrepresented students. Ultimately, organizations need to incentivize this type of diversity and inclusion work through hiring, pay, and promotion.
To diversify the pipeline, the second proposed strategy in MAPS is academic exposure. In most medical schools, a clinical rotation in cardiology is not a component of the core curriculum, and electives are offered during fourth year. In one study, elective exposure to cardiology during preclinical years increased the likelihood of students pursuing the field. We believe both preclinical and clinical exposure can be integrated into current training paths. At the preclinical level, offering continuity clinics within cardiology can engage students with real-world experience. During the clinical years, cardiology electives can be integrated within the internal medicine clerkship by offering at least 1 week of subspecialty exposure. In addition, funded cardiology elective programs (eg, Johns Hopkins pediatric cardiology elective) for students underrepresented are crucial to diversify the pipeline.
We recognize that not all students have access to a home cardiology program or may be unable to fit an elective into their schedule. The COVID-19 pandemic has uncovered new forms of learning, including simulation technology, free open-access medical education, and social media. For example, ultrasound simulation, clinical problem-solving sessions, podcasts, webinars, and virtual grand rounds offer remote alternatives to remain engaged. We believe students, who have increasingly used asynchronous learning during the preclinical curriculum, would benefit from self-directed, self-paced content designed by professional societies or third parties. Much of this content exists but requires repurposing and standardization for students. We understand that technology can exacerbate disparities in knowledge in other domains. However, providing free resources to students may help increase access and reduce disparities in knowledge.
The third proposed strategy in MAPS to diversify the pipeline is professional development outside of medical school. The MSLG has invited students to collaborate with the ACC Fellows-in-Training Council to create summary slides for clinical trials presented at the American Heart Association 2020 Scientific Sessions. It has also formed a research program consisting of 60 students to publish systematic reviews in collaboration with ACC faculty members. It has created a directory of cardiology interest groups and curated the ACC Member Hub platform, with >200 registered trainees, to promote relevant programming. These types of joint initiatives have taught us it is possible to formalize and democratize professional development, especially for international students and those without home cardiology programs.
The ACC, American Heart Association, and ABC have existing programs in the professional development space to increase minority recruitment. Several years ago, the ACC Task Force on Diversity and Inclusion created the Young Scholars Program, which gives high school and college students an opportunity to attend an annual conference. Last year, the ACC Task Force convened a similar program for internal medicine residents. However, a gap exists at the medical student level where, despite scholarships, no large professional development program exists. We believe that organizations should collaborate with culturally focused organizations such as the Latino Medical Student Association and ABC to address gaps and provide resources for URiM students. Over the long term, this collaboration may increase involvement from trainees within these societies. Although professional development programs at the student level are important, interventions upstream are also needed. Medical school classes require greater diversification through holistic review for admissions to increase URiM matriculants.
The fourth proposed strategy in MAPS to diversify the pipeline is a support network. Students can leverage professional societies or social media platforms such as Twitter to identify role models at other institutions. Several well-known initiatives that highlight the hashtag activism in this space include #TakeAWomanToTheCathLab, #BlackMenInMedicine, and the CardioNerds Narratives in Cardiology series. Cardiologists who are willing to share the personal challenges they overcame during training can allow students to gain a sense of belonging within the field. We believe that involving students through these initiatives can help address barriers and misconceptions while answering common questions related to work–life integration. However, a challenge with implementing support networks at the medical student level includes the lack of a central organization to coordinate students. To allow members to share their personal journey and for students to find a support network, the ACC MSLG has had several initiatives, including the Perspective Piece and Member Spotlight platforms.
In summary, we advocate for a 4-part strategy to diversify the training pipeline into cardiology that leverages our MAPS paradigm: meaningful mentorship, academic exposure, professional development, and a support network. We view our role as leaders of the MSLG to build and sustain medical student interest in cardiology. However, we recognize that we are still limited in our reach, and that to address growing disparities, we will need more institutional and professional support. In the next decade, we look forward to the implementation of these strategies to make cardiology a more inclusive professional home for all.
This article is reproduced from JACC journals.
Surgerycast
Shanghai Headquarter
Address: Room 201, 2121 Hongmei South Road, Minhang District, Shanghai
Tel: 400-888-5088
Email: surgerycast@qtct.com.cn
Beijing Office
Address: room 709, No.8, Qihang international phase III, No.16, Chenguang East Road, Fangshan District, Beijing
Tel: 13331082638(Liu Jie)
Guangzhou Office
Address: No. 15, Longrui street, longguicheng, Taihe Town, Baiyun District, Guangzhou
Tel: 13302302667