Dynamic Perfusion With CT Angiography: Adding Another Feather to a Heavily Decorated Cap
The most appropriate diagnostic algorithm for patients with stable coronary artery disease (CAD) is still an unresolved matter of debate. Anatomical imaging of the coronary arteries using coronary computed tomography angiography (CTA) carries very high negative predictive value in low- to intermediate-risk patients and, especially when performed with recent generation of scanners, is associated with low radiation exposure, allowing for it to be the first test to rule-out CAD. However, the setting of patients with known or previously revascularized CAD is significantly more complex, challenging the role of noninvasive anatomical coronary imaging. In these patients, additional information about functional importance of CAD could be more useful, at least for explanation of the change in symptomatic status.
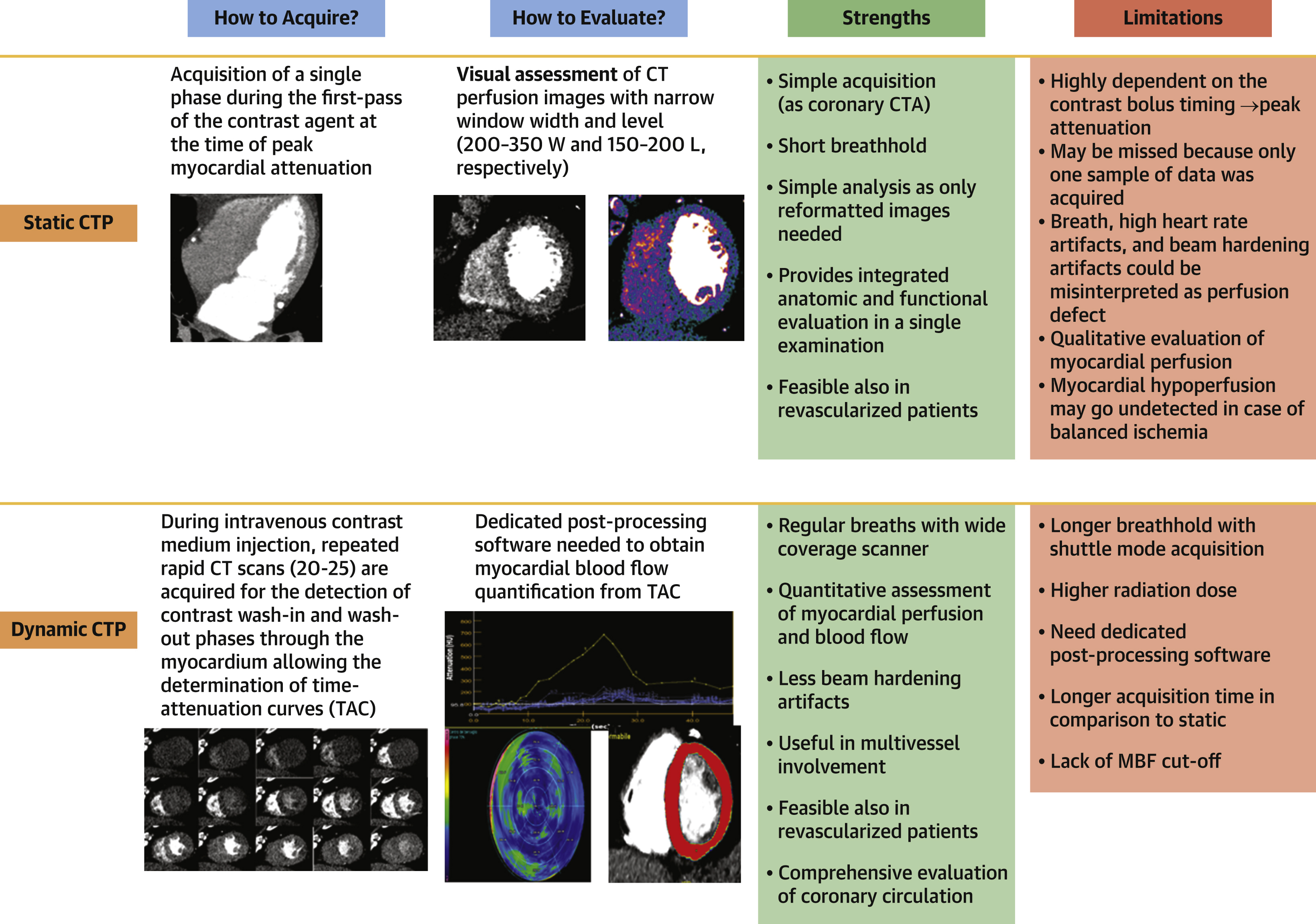
Computed tomography myocardial perfusion (CTP) imaging offers a comprehensive tool for the evaluation of patients with stable chest pain, providing information on coronary atherosclerosis and myocardial perfusion during the same session. CTP has been validated against a combination of invasive coronary angiography and single-photon emission computed tomography (CT) (7), stress cardiac magnetic resonance, or invasive FFR. In contrast to the static CTP that is based on acquisition of a single phase during the first pass of the contrast agent, the dynamic CTP relies on acquisition of multiple samples of the same volume of myocardium over time to construct time-attenuation curves. With application of different mathematical models, myocardial blood flow (MBF) and other perfusion parameters are then calculated from time-attenuation curves. Dynamic CTP can be performed either using a CT scanner with full heart coverage within 1 gantry rotation or using a dual-source CT system with the shuttle-mode technique to cover the entire heart. The post-processing phase employing semiautomatic software allows quantification of MBF that is expressed as min/100 ml/min for each of the 16-segment heart model. Figure 1 shows the technical differences, strength, and limits of static and dynamic CTP.
CT Perfusion
Although attractive, perfusion CT has struggled to find a place in routine clinical practice for a number of reasons, including concerns about the radiation dose and prolonged examination table time, lack of availability of the latest CT technology and adequate software tools for CT perfusion image analysis, reluctance to employ vasoactive drugs and uncertainty about perfusion imaging protocols, and the need for both cardiological and radiological competences to perform an examination safely.
In this issue of the Journal, Kitagawa et al report a multicenter observational study testing the diagnostic accuracy of the combination of coronary CTA plus stress dynamic CTP plus delayed enhancement acquisition against the reference standard of invasive evaluation with FFR. They enrolled 157 patients undergoing a clinically indicated invasive coronary angiography (ICA) and referred them for the combined CT protocol. They report a significant improvement of accuracy with combined protocol compared with coronary CTA alone: the area under the curve improved from 0.65 to 0.74. The dynamic CTP was particularly useful when multivessel disease was suspected on coronary CTA. Furthermore, among the 157 patients, 54 (34%) had known CAD including a history of myocardial infarction and percutaneous coronary intervention with previous coronary artery stent placement in 30% of patients. This study confirmed as others the usefulness of the combined protocol even in revascularized patients. In terms of clinical applicability, CTP was considered comparable to the CT-derived fractional flow reserve.
Quantification of MBF is of fundamental importance for the diagnosis of myocardial ischemia in case of multivessel disease, where extensive but balanced ischemia might be underestimated. Kitagawa et al underscored that the improved diagnostic performance with dynamic CTP was particularly evident when multivessel disease was discovered by coronary CTA. The addition of dynamic CTP to coronary CTA significantly increased area under the curve from 0.80 to 0.84 (P = 0.04) in 2-vessel disease and from 0.65 to 0.73 (P = 0.02) in 3-vessel disease, but not so in 1-vessel disease (from 0.84 to 0.87; P = 0.265).
Despite growing evidence for the diagnostic accuracy of CTP, a robust cutoff value for hyperemic MBF that allows identification of hemodynamically relevant stenosis is lacking. In this paper, absolute MBF value as well as those normalized by remote MBF, which was the highest MBF among the 16 segments, were used to assess myocardial perfusion (relative MBF values). The authors report that the optimal cutoff value for hemodynamically significant stenoses was 116 mL per 100 mL/min in absolute MBF or 0.71 in relative MBF, both in all vessels and in vessels with ≥50% stenosis on coronary CTA. The total radiation dose of the whole CT in this study was 12.8 ± 4.3 mSv, higher than that reported in another studies and higher than the average dose delivered from single-photon emission CT (10.48 mSv) and from diagnostic ICA (11.6 mSv) in the CORE320 (Combined Non-invasive Coronary Angiography and Myocardial Perfusion Imaging Using 320 Detector Computed Tomography [CORE320]) trial possibly because of the acquisition of delayed enhancement phase. The authors did, however, demonstrate that the diagnostic performance of dynamic CTP was not improved by addition of the information obtained from the delayed enhancement and that the late enhancement phase can be conveniently obviated. The futility of delayed enhancement could be because of lower MBF within the viable myocardium around scar compared with the remote myocardium.
In this paper, the reference standard was the use of ICA with invasive FFR that only addresses the stenosis of the epicardial vessels and overlooks the importance of endothelial function, microcirculation, and so on, which could influence myocardial blood supply. Dynamic CTP offers an approach to evaluate the entire cascade of the myocardial perfusion, which translates into a true functional test. This could be particularly important in women and diabetic patients in whom microcirculatory disease could contribute to chest pain.
We believe that the dynamic CTP might be regarded as a worthy partner for coronary CTA, which already provides substantial information about anatomic stenosis, fractional flow reserve, and plaque morphology. CTP would likely find an ideal role in moderate, diffuse multivessel coronary lesions in patients with established disease or already revascularized, to help physicians better triage patients and reduce potential over-referral for myocardial revascularization after routine coronary CTA. Other technological improvements are needed to reduce radiation dose for more widespread clinical application. However, multicenter and multivendor cost-effectiveness studies would be required to define clinical indication for addition of dynamic myocardial CTP imaging to the protocol..
This article is reproduced from JACC journals.
surgerycast
Shanghai Headquarter
Address: Room 201, 2121 Hongmei South Road, Minhang District, Shanghai
Tel: 400-888-5088
Email:surgerycast@qtct.com.cn
Beijing Office
Address: room 709, No.8, Qihang international phase III, No.16, Chenguang East Road, Fangshan District, Beijing
contact number:010-5123-5010 13331082638(Liu Jie)