Treating Bifurcation Lesions: The Result Overcomes the Technique
The final luminal cross-sectional area at the ostium of the side branch may predict the outcome of 2-stent techniques, provided the main branch luminal cross-sectional area is kept optimal. This simple statement is not meant to highlight that the 2-stent technique is the best approach anywhere, anytime. Indeed, plenty of studies have demonstrated that, when possible, placing a single stent on the main branch, with or without side branch opening, is the preferred approach when treating a bifurcation lesion. Similarly, recent evidence revealed comparable results with stepwise provisional and systematic dual stenting in true left main bifurcation lesions. Nevertheless, there are situations in which a 2-stent technique (main and side branch) should be implemented as intention-to-treat, so that lesion stratification is key before stenting technique selection. The left main bifurcation lesion depicted in Figure 1 is, in our view, a typical lesion difficult to treat with a single stent, for which the philosophy of ″less is more″ may not be the most convenient.

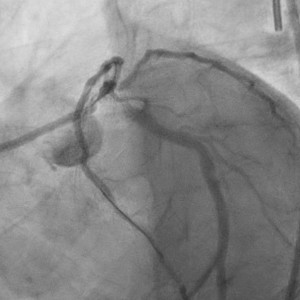
Complex Coronary Bifurcation Lesion
Complex true left main Medina 1-1-1 coronary bifurcation lesion including shaft and distal left main stem, long left anterior descending coronary artery disease extending into an early diagonal branch and ostioproximal left circumflex artery, with bifurcation angle >70°.
The concept leading to the development of crush stenting (CS) was to effectively stent the side branch at the same time as main branch stenting. At the time when CS was initially developed, this approach provided, differently from any other 2-stent technique, immediate patency of both the main and side branches. This attribute is relevant only in particular settings such as severe stenosis on the main and side branches (usually left main) with acute coronary syndrome (Figure 2). Raphael et al discuss, in their review in this issue of JACC: Cardiovascular Interventions, how CS evolved into more refined iterations. The double kissing (DK) crush represents today the most advanced technique for the intention-to-treat approach with 2 stents and is supported by the largest amount of published evidence. Indeed, very promising results were reported in the DEFINITION-II (Two-Stent vs Provisional Stenting Techniques for Patients With Complex Coronary Bifurcation Lesions) trial (7), enrolling patients with complex coronary bifurcation lesions, in which a 2-stent technique (mainly DK crush) was associated with more than halving of both target vessel myocardial infarction and target lesion revascularization incidence at 1 year compared with provisional stenting.

Settings in Which the Original Crush Technique May Be Advantageous
Acute coronary syndrome with evidence of severe left main trifurcation disease extending into proximal left anterior descending and circumflex coronary arteries.
The main questions addressed in this review are the following: 1) What are the real advantages of CS versus culotte stenting? 2) What is the modern CS, and is DK crush a must? and 3) Should we keep alive other techniques, such as T stenting or T and protrusion?
The DKCRUSH-III (Double Kissing [DK] Crush Versus Culotte Stenting for the Treatment of Unprotected Distal Left Main Bifurcation Lesions) randomized trial comparing DK crush versus culotte stenting reported advantages for DK crush, even though many experienced operators do not fully agree with these results. The 3-year results of the Nordic Stent Technique Study (8) did not report a difference between culotte stenting and CS, although it is important to note that in that study, operators did not perform DK when using CS. As pointed out in the present review, culotte stenting may have limitations when the angle between the main branch and side branch is close to 90° and when a large discrepancy between the sizes of the main and side branches is present. Therefore, DK crush may not have clear advantages compared with culotte stenting, provided culotte stenting is not used in bifurcation lesions with the unfavorable characteristics outlined earlier.
Regarding modern CS, minimal overlap in the main vessel should be achieved. For this reason, the mini-CS approach should be followed, while nano-CS, prone to risk for missing the side branch ostium, should be avoided.
The advantage of DK crush derives from performance of kissing balloon inflation twice, facilitating optimal apposition of the struts at the carina and permitting a more friendly recrossing into the side branch. The combination of well-performed proximal optimization and single high-pressure noncompliant balloon inflation may yield similar results, but these details are outside the aims of a randomized study.
Other techniques, such as T stenting and T and protrusion, are valuable when the angle between the main and side branches is close to 90° and should be used taking advantage of the simplicity and absence of need for stent recrossing.
The main emphasis should be on lesion preparation. Indeed, a fundamental objective of any 2-stent technique is achievement of an adequate lumen at the ostium of the side branch, which is the ″weak spot″ in this context.
The role of imaging, when performing a 2-stent technique, becomes essential. It is not rare to perform an additional kissing inflation (3 times kissing) when intravascular ultrasound (IVUS) or optical coherence tomography evaluations show a suboptimal result. Of note, IVUS use in the DKCRUSH-V trial was relatively low (42%); more widespread use of this technology might have positively influenced outcomes (especially for more complex lesions), even though subgroup analyses revealed superimposable benefit of DK crush versus provisional stenting in IVUS- and angiography-guided procedures.
After so many efforts to fully refine this field, the ingredients for optimal bifurcation stenting when 2 stents are needed can be summarized as follows (Figure 3): 1) optimal lesion preparation; 2) stenting with DK crush and minimal overlap or culotte or T stenting when appropriate; 3) evaluation with imaging of results after lesion preparation and after stenting (this step may not be easy after T stenting); and 4) further dilatation, if needed.

The Role of the Crush Technique in a Complex Coronary Bifurcation Lesion Requiring a 2-Stent Technique
The main criteria favoring a 2-stent technique are outlined. Nonetheless, the decision to undertake intervention according to such a strategy may be taken following predilation of main and side branches. DK = double kissing.
The published research on stenting bifurcation lesions is so broad that supporting data can be found for almost any approach. It is therefore difficult not to be biased and opinionated. Nevertheless, some practical statements should remain: 1) the operator must remember that any 2-stent technique with a suboptimal result exposes the patient to thrombosis and restenosis; 2) treating the side branch with a drug-coated balloon is an emerging approach; and 3) the final result is far more important than the technique used.
This article is reproduced from JACC journals.
surgerycast
Shanghai Headquarter
Address: Room 201, 2121 Hongmei South Road, Minhang District, Shanghai
Tel: 400-888-5088
Email:surgerycast@qtct.com.cn
Beijing Office
Address: room 709, No.8, Qihang international phase III, No.16, Chenguang East Road, Fangshan District, Beijing
contact number:010-5123-5010 13331082638(Liu Jie)