Warfarin Is the Preferred Therapy for Patients With Thrombotic APS: Back to the Future
Thrombotic antiphospholipid syndrome (APS) is an autoimmune disorder that is challenging to diagnose and treat correctly. A correct diagnosis requires clinical manifestations (venous, arterial, or placental thrombosis) and laboratory criteria documented on at least 2 occasions at least 12 weeks apart. These patients are generally considered to be at high risk for recurrent thrombosis and require indefinite-duration anticoagulation therapy.
Direct oral anticoagulants (DOACs) are eclipsing vitamin K antagonists (VKAs) as the preferred agent for venous thromboembolism because of their ease of use and safety. DOACs are an attractive alternative to warfarin in patients with APS, but several small randomized controlled trials have indicated that DOACs may be associated with worse outcomes than VKAs, especially in those patients with high-risk APS features such as triple positivity and prior arterial thrombosis.
Some evidence-based guidelines have supported the use of DOACs as alternatives to VKAs in certain “non–high-risk” APS patients, including single- or double-positive serology in patients unwilling to undergo International Normalized Ratio monitoring or with poor therapeutic International Normalized Ratio control. However, available trials were relatively small and not sufficiently powered to assess thrombotic outcomes or analyze critical subgroups. Clinicians, therefore, remain uncertain about the treatment tradeoffs between DOACs and VKAs in patients with non–high-risk types of thrombotic APS. In this issue of the Journal of the American College of Cardiology, Khairani et al present the results of their systematic review and meta-analysis comparing the efficacy and safety of DOACs with VKAs in patients with thrombotic APS. Their results clarify clinical decision-making for patients with thrombotic APS but also raise questions that highlight the need for continued research to optimize care in this challenging patient population.
Khairani et al asked whether VKA or DOAC is preferred in patients diagnosed with thrombotic APS. They followed accepted systematic review and meta-analysis standards, including using risk of bias and reporting quality assessments. The treatment effect of DOACs vs VKAs was explored in important high-risk subgroups, including patients with high-risk serology (“triple-positive APS”) and those with previous arterial thrombotic events. Four open-label, randomized, controlled trials—from the United Kingdom, Italy, Spain, and the United States, comprising 474 patients with confirmed thrombotic APS—were included in the analysis (240 treated with VKA and 234 with DOACs). Compared with VKAs, DOACs were associated with significantly increased odds of arterial thrombotic events (OR: 5.43; 95% CI: 1.87-15.75), especially stroke, whereas there was no change in the odds of venous thrombotic events (OR: 1.20; 95% CI: 0.31-4.55) or major bleeding (OR: 1.02; 95% CI: 0.42-2.47). Subgroup analysis by type of APS (triple positive vs single/double positive), and history of arterial thrombosis did not affect the increased odds of arterial thrombosis associated with DOACs compared with VKAs. Similarly, odds of the other outcomes were not modified in the subgroup analysis.
As the quality of the evidence was rated “high” for the arterial thrombosis outcome and “moderate” for the venous thrombosis and bleeding outcomes, these results should lead to a revision of evidence-based guidelines to recommend against using DOACs as an option for most patients with thrombotic APS. This recommendation for VKAs also applies to patients previously thought to be at lower risk from APS—including those with only 1 or 2 positive serological tests and those with only prior venous thrombosis.
This clarification of existing recommendations will have important implications for clinicians. Given the heightened consequences of an APS diagnosis on anticoagulation therapy choice, the diagnosis of APS must be made accurately, including confirmation and documentation of positive laboratory tests at least 12 weeks after the initial positive test. While awaiting confirmatory APS testing, patients with suspected APS should avoid DOACs. Strong consideration should be given to switching essentially all APS patients currently receiving DOACs to VKAs. Shared decision-making can be considered in rare circumstances with respect to the use of other agents; however, shared decision-making is best used when there is clinical equipoise, which now does not apply to many patients with APS and prior thrombosis.
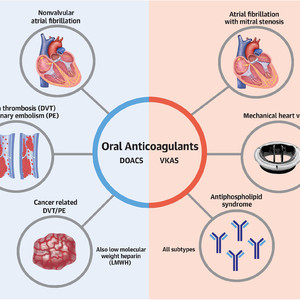
DOACs have been an important advance in preventing and treating thrombotic disease. However, there is a growing list of situations where DOACs appear less effective than VKAs (Figure 1). That list now includes most patients with thrombotic APS,12 mechanical heart valves, and atrial fibrillation associated with rheumatic valvular disease. Why DOACs are less effective than VKAs in certain circumstances (but superior in others) requires further explanation, but may include the fact that in patients at higher risk of thrombosis, targeted inhibition of a single clotting factor may not be sufficient to provide adequate suppression of the clotting factor cascade.

Current Evidence-Based Indications for Warfarin or Other Anticoagulant Medications
Warfarin, the standard oral coagulant for over 50 years, has been supplanted for many indications by direct oral anticoagulants (DOACs). However, there remain several evidence-based indications for warfarin in preference to the DOACs, in addition to those patients who take warfarin because of personal preference or cost considerations. DOACs are preferred because of their simplicity of use, lack of need for monitoring, and much-reduced concerns for drug-drug interactions. However, there is clear evidence from patients with antiphospholipid antibody syndrome, mechanical heart valves, and now rheumatic valvular disease that warfarin is preferred to DOACs based on enhanced safety and/or efficacy.
This article is reproduced from JACC journals.
Surgerycast
Shanghai Headquarter
Address: Room 201, 2121 Hongmei South Road, Minhang District, Shanghai
Tel: 400-888-5088
Email: surgerycast@qtct.com.cn
Beijing Office
Address: room 709, No.8, Qihang international phase III, No.16, Chenguang East Road, Fangshan District, Beijing
Tel: 13331082638( Liu )
Guangzhou Office
Address: No. 15, Longrui street, longguicheng, Taihe Town, Baiyun District, Guangzhou
Tel: 13302302667 ( Ding )