Optimizing Blood Pressure Components for a Healthy Brain: The Holy Grail in Blood Pressure Management
The number of adults with elevated blood pressure (BP) has doubled over the past 3 decades, and hypertension is among the leading modifiable risk factors for attributable deaths. The association between hypertension and cardiovascular events, even in young and middle-aged adults, has been firmly established. Although less explored, the relationship between high BP and cognitive decline and dementia has attracted attention in recent years. Recent observational studies suggest that cumulative BP levels are directly associated with faster cognitive decline and a higher risk for incident dementia later in life. Similarly, exposure to elevated BP from childhood and young adulthood is associated with worse midlife cognitive performance. Most previous studies have focused on systolic BP (SBP) or single–time point BP measures, with only very few addressing the association between cumulative exposure to different BP components and cognitive impairment.
In this issue of the Journal of the American College of Cardiology, Li et al use longitudinally collected data from almost 17,000 cognitively healthy adults ≥50 years of age included in the HRS (Health and Retirement Study) and ELSA (English Longitudinal Study of Ageing) to examine the effects of cumulative exposure to different BP components on cognitive decline, incident dementia, and all-cause mortality. The investigators found that higher cumulative SBP and pulse pressure (PP) were independently associated with accelerated global cognitive decline, elevated risk for dementia, and increased all-cause mortality. In contrast, diastolic BP (DBP) showed a significant inverse association with clinical outcomes. Although the HRS and ELSA populations differ in their baseline characteristics, a battery of sensitivity analyses produced consistent results across both cohorts.
Given the observational nature of the study, there is potential for unmeasured confounding, and clinical interpretation of the results is difficult because of the way cognitive scores are standardized and the use of cumulative BP values; nevertheless, the study by Li et al presents important findings highlighting the potential for different BP components to have distinct impacts on cognitive outcomes.
The detrimental effect of long-term elevated SBP on cognitive outcomes and mortality is in line with previous studies. The opposite trend found for DBP is intriguing and may be related to a reported J-shaped relationship between DBP and cardiovascular events. These studies found that not only high but also very low DBP is detrimental, with values <70 mm Hg, and especially <60 mm Hg, associated with impaired myocardial perfusion, subclinical myocardial damage, and increased risk for cardiovascular events. The inverse correlation between DBP and cognitive decline found by Li et al may thus arise from the combination of low DBP and impaired cerebrovascular autoregulation in patients with chronic hypertension, which can lead to insufficient cerebral tissue perfusion.
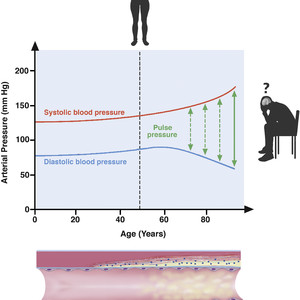
PP is easily measured as the difference between SBP and DBP, but its impact on cognitive outcomes has been barely studied. PP widening is a normal consequence of aging. Both SBP and DBP increase until the age of 55 years, after which they diverge as diastolic pressures decrease and systolic pressures continue to rise (Figure 1). The hemodynamic physiology of age-related wide PP and systolic hypertension might be a consequence of the gradual degenerative stiffening of arteries due to atherosclerosis, which reduces the compliance of the central arterial system. This arterial stiffening increases the proportion of flow occurring during systole, resulting in elevated SBP. In parallel, the loss of arterial compliance prevents BP increases during diastole, and DBP therefore falls. The biomechanical hypothesis of brain damage proposes that cognitive decline originates mainly from PP-induced microvascular damage. The increase in PP generates mechanical stress in the fragile brain microcirculation, causing hypertrophy of the cerebral vascular arterial wall. Persistent exposure to pulsatile stress results in white-matter damage, lacunas, brain atrophy, and loss of cortical connections, thus affecting cognitive performance.

Association of Blood Pressure Components With Cognitive Impairment
In the absence of effective targeted pharmacologic treatments to delay cognitive impairment or slow the progression of dementia, researchers have focused on controlling modifiable risk factors such as hypertension. A recent meta-analysis of randomized clinical trials demonstrated that compared with control, BP lowering with antihypertensive agents was significantly associated with a lower risk for incident dementia or cognitive impairment.
Pulling these threads together, in middle-aged and older people, it seems reasonable to control long-term SBP and simultaneously maintain adequate DBP. International guidelines on hypertension management suggest a less strict BP target for patients aged ≥65 years, particularly frail or dependent patients, and patients with postural hypotension. However, the guidelines barely mention PP, which might be particularly relevant to the hypertension-mediated organ damage in middle-aged and older people.
Although one size does not fit all, on the basis of recent data, we could propose a target SBP of 110-130 mm Hg for this population, paired with a target DBP of 70-80 mm Hg to maintain appropriate PP, avoid hypotension, and reduce both cardiovascular events and cognitive decline and dementia. Nevertheless, there is a need for additional long-term large observational studies and randomized trials to define optimal BP component and PP values. In the near future, wearable devices may provide a valuable and convenient way to obtain granular, population-level data on the lifetime impact of cumulative BP components and other health factors and behaviors on cardiovascular and cognitive outcomes later in life. In the meantime, beyond pharmacologic BP control, efforts should focus on health promotion programs directed at all age groups, particularly children and young adults, with the aim of preventing hypertension and other modifiable risk factors from appearing in the first place, in order to maintain a long-lasting healthy brain.
This article is reproduced from JACC journals.
surgerycast
Shanghai Headquarter
Address: Room 201, 2121 Hongmei South Road, Minhang District, Shanghai
Tel: 400-888-5088
Email:surgerycast@qtct.com.cn
Beijing Office
Address: room 709, No.8, Qihang international phase III, No.16, Chenguang East Road, Fangshan District, Beijing
contact number:13331082638(Liu Jie)