Peripheral Matters | COVID-19 and the Risk of Thrombosis: Insights from the CORONA-VTE Registry
Since the early days of the COVID-19 pandemic, concerns have been raised regarding the arterial and venous thrombotic complications of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection.These include myocardial infarction, ischemic stroke and venous thromboembolism.
A body of evidence has since accumulated and patients with COVID-19 who are admitted to the intensive care unit (ICU) appear to be at highest risk.The mechanism for these events is thought to be multifactorial, including a prothrombotic state and direct endothelial injury by SARS-CoV-2.Given the mounting evidence, experts initially recommended thromboprophylaxis for hospitalized patients with COVID-19.However, early reports of these complications were limited by small sample size and heterogeneity in event definitions. More recently a U.S. based multicenter registry of COVID-19 patients was established to better understand the arterial and venous thrombotic complications of SARS-CoV2 infection.
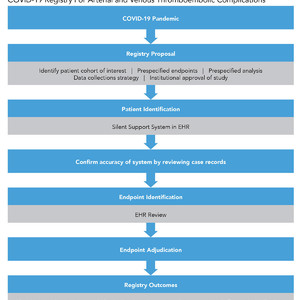
The registry, CORONA-VTE (COVID-19 Registry to Assess Frequency, Risk Factors, Management, and Outcomes of Arterial and Venous Thromboembolic Complications), was established in 2020 to evaluate patients with COVID-19, based on a positive polymerase chain reaction (PCR) test and COVID-19 related respiratory symptoms, for arterial and venous thromboembolic disease (Figure 1). Patients were identified through a silent computerized decision support program embedded in an electronic health record (EHR) that identifies eligible patients. The 100% accuracy of this program was confirmed by reviewing the records of each patient in the registry. The registry includes patient demographics, cardiovascular disease and risk factors status, disease-specific management, and 30-day cardiovascular outcomes including arterial and venous thromboembolism and bleeding events. Outcome events were identified by an extensive review of the EHR for each participant. An independent clinical endpoint committee composed of three cardiovascular medicine specialists was established to adjudicate these events.

The first report from this registry was published in the Journal of the American College of Cardiology in November 2020.In this report, the authors included 1,114 consecutive patients who were >18 years old and stratified according to admission status (170 admitted to ICU, 229 admitted to non-ICU, 715 in outpatient setting). Five key findings come from this study.
One, major arterial and venous thromboembolism occurred in 35.3% of patients admitted to an ICU, 2.6% of those admitted to non-ICU, and 0% of those in the outpatient setting. Two, catheter- and device-related deep vein thrombosis (DVTs) accounted for the majority of DVTs in this study (76.9%). Three, thromboprophylaxis in the form of anticoagulation was prescribed in 89.4% of patients admitted to an ICU and 84.7% of those admitted to a non-ICU. Four, among patients admitted to an ICU, acute respiratory distress syndrome (ARDS) was associated with a seven-fold increase in odds of major arterial and venous thromboembolism (odds ratio, 6.68; 95% confidence interval, 1.85-24.14). Five, symptomatic venous thromboembolism occurred in 27% of patients admitted to an ICU and 2.2% of patients admitted to a non-ICU.
Findings from this initial report are consistent with those from the global community, with patients in the ICU being at particularly high risk despite the use of prophylactic anticoagulation. In particular, ARDS was noted to be an important predictor of major arterial and venous thromboembolism. This likely reflects the underlying severity of COVID-19 and the hyperinflammatory state that occurs. This leads to a hypercoagulable state seen in many patients in the ICU and potentially explains the high rate of catheter- and device-related DVTs seen in this cohort. However, despite patients in the ICU being at particular risk, patients with COVID-19 admitted to a non-ICU setting were also at risk of arterial and venous thromboembolism. The estimations from the CORONA-VTE registry likely underestimate the burden as systematic venous thromboembolism screening was not instituted in this cohort. However, evidence-based practice guidelines do not recommend systematic screening for asymptomatic DVT and the clinical significance of these remains the subject of vigorous debate.
The CORONA-VTE registry has shed light on the high incidence of major arterial and venous thromboembolism. Since its initiation, several studies have reported their results on the outcomes of various anticoagulation strategies in patients with COVID-19 and many more studies remain ongoing (Table 1). For example, the Intermediate vs. Standard-Dose Prophylactic Anticoagulation in Critically ill Patients With COVID-19: An Open Label Randomized Controlled Trial (INSPIRATION) trial showed no significant benefit with intermediate dose prophylactic anticoagulation compared with a standard dose in patients admitted to the ICU.

The preliminary, non-peer reviewed results of a multiplatform randomized control trial of three international trials evaluating the role of higher doses of prophylactic anticoagulation in hospitalized patients does not show a benefit in patients admitted to the ICU but some benefit in those admitted to a non-ICU setting for the primary outcome (organ-support free days).The three international trials included in this multiplatform study were the Randomized, Embedded, Multi-factorial Adaptive Platform Trial for Community-Acquired Pneumonia (REMAP-CA) study, Accelerating COVID-19 Therapeutic Interventions and Vaccines-4 (ACTIV-4) study, and Antithrombotic Therapy to Ameliorate Complications of COVID-19 (ATTACC) study.
The findings from the multiplatform study have not been cited by any national society guidelines. However, on February 8, 2021, the American Society of Hematology published a recommendation against using higher doses of anticoagulation (intermediate or full) in patients with COVID-19-related critical illness.
In summary, as studies like the CORONA-VTE registry continue to improve our understanding of these events, future studies will focus on evaluation of risk stratification and prevention strategies in a real-world cohort.
This article was authored by Zaid Almarzooq, MBBCh, a fellow in training in cardiovascular medicine at Brigham and Women’s Hospital, and Gregory Piazza, MD, MSc, FACC, director of vascular medicine at Brigham and Women’s Hospital and associate professor of medicine at Harvard Medical School, all in Boston, MA.
surgerycast
Shanghai Headquarter
Address: Room 201, 2121 Hongmei South Road, Minhang District, Shanghai
Tel: 400-888-5088
Email:surgerycast@qtct.com.cn
Beijing Office
Address: room 709, No.8, Qihang international phase III, No.16, Chenguang East Road, Fangshan District, Beijing
contact number:010-5123-5010 13331082638(Liu Jie)